Fentanyl is 50 times stronger than heroin and 100 times more potent than morphine. Owing to the great deal of variation in the sensitivity of each person, and its potency, fentanyl is a real danger to human health if not used as prescribed or appropriately.
A lethal dose of fentanyl looks and weighs the same as just a few grains of sand
Deaths from fentanyl overdose have been on the rise worldwide. The UK reported a 29 per cent increase in fentanyl-related deaths from 2016 to 2017 and in the same period the US reported an alarming 45.2 per cent increase. In Australia synthetic opioid related deaths (e.g. tramadol and fentanyl) are also on the rise, from 2007 to 2016 there has been a 1,082 per cent increase. In 2016 there were 214 deaths or 1.3 deaths per 100,000 people, an increase from 0.11 per 100,000 in 2007.
Given its potency it's no surprise that the majority of fentanyl-related deaths worldwide are reportedly accidental. Fentanyl has been associated with the untimely deaths of musical legends Prince and Tom Petty, both of whom were prescribed the drug for severe and chronic pain.
The therapeutic indication for fentanyl is severe pain, in particular from cancer in the terminal (palliative) phase. Misuse, unsafe increases in dosage and combining with other medicines that cause sedation, such as sleeping tablets, increase the risk of harm and death from fentanyl.
How prescription fentanyl overdose occurs
In Australia fentanyl can be prescribed in the form of transdermal patches, lozenges or intravenous injection. Because the difference between a therapeutic dose and a fatal dose is so small, people who self-administer prescribed fentanyl products are at a greater risk of overdose and therefore should use with extreme caution.
Overdose can occur through easy mistakes such as lapses in keeping track of how much and how often it is being taken. Fatal overdose can happen when a patient applies an additional patch without removing the last, applies heat to the patch, or takes too many lozenges too close together. There is also the danger of the products getting into the hands of people without a prescription, for instance access by others in the home including family, friends, or children.
As far back as 2006 the NSW Therapeutic Advisory Group (TAG) alerted health services to a number of safety warnings following reports of deaths and adverse reactions in patients overseas using fentanyl skin patches. An elderly patient died following application of a heat pack over a patch, a child died after applying one of his mother's patches on himself and several children escaping near death applying patches to themselves.
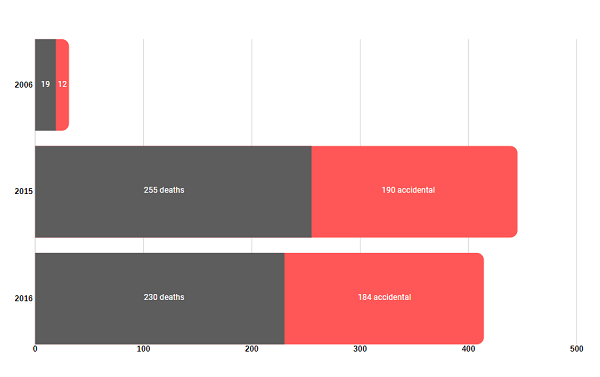
Synthetic opioid overdose in Australia
76 per cent of the Australians who died of an opioid overdose in 2016 did so using pharmaceutical opioids, according to a report released by the National Drug and Alcohol Research Centre (NDARC) at UNSW. The NDARC report also shows that the rate of opioid-related deaths has almost doubled over the last ten years. Tragically, 85 per cent of all opioid-induced deaths were considered accidental.
Synthetic opioid deaths in Australia
(Synthetic opioid analgesics include fentanyl, tramadol and pethidine)
Overdose in the illicit drug market
Owing to its potency, illegal drug producers can distribute large quantities of fentanyl which they then mix into other drugs with little to no precision. Meaning, users injecting heroin or inhaling other drugs laced with fentanyl won't know they're taking a lethal dose until it's too late.
Last year celebrity singer Demi Lovato opened up about her alleged near death from consuming a drug laced with fentanyl. This highly publicized event demonstrates the risk to recreational drug users of any economic or social status, and how it's almost impossible to know what's in a drug manufactured illegally.
Although an overdose can occur by any route of administration (dermal, oral, smoked, snorted or injected), it is particularly likely with intravenous use (syringe). Fentanyl can also be particularly dangerous if used with alcohol, sleeping tablets, antidepressants or antianxiety medication (e.g. benzodiazepines) or if already intoxicated with another drug.
Signs of fentanyl overdose
There is a very real risk of overdose from fentanyl when used other than by your doctor's instructions, this is due to its potency and very fast action once inside the body. It is never safe to inject the contents of a fentanyl patch, but if you do so, make sure a friend is always with you.
Signs of overdose may include:
- Rapid onset of difficult, shallow or slow breathing – fentanyl often makes people stop breathing
- Confusion
- Fainting
- Cold and clammy skin and low body temperature
- Bluish skin and nails, because of low oxygen
- Coma and death
What to do in an emergency
Always phone
000 (triple zero) for an ambulance and tell the operator that the person has overdosed.
DO:
- Try not to panic
- Stay with the person
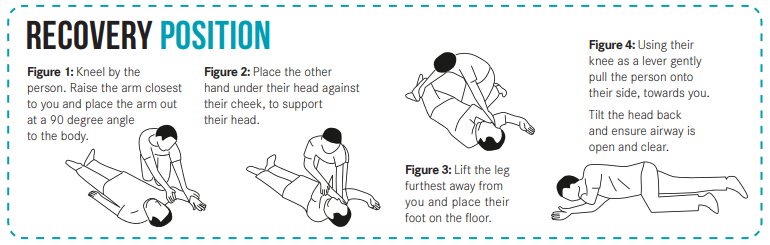
- If they are unconscious, put them on their side in the
recovery position
- Check their breathing, clear their airway
- Do mouth-to-mouth resuscitation if they have stopped breathing
- Administer opioid overdose reversing medicine, naloxone.
Access Take Home Naloxone for free from your local pharmacist. For more information visit yourroom.health.nsw.gov.au/naloxone.
DO NOT:
- Inject the person with any other illicit drug
- Put them under the shower
- Put anything in their mouth as it can cause them to choke and stop breathing.
Even if someone fits (has a seizure or convulsion), the best thing to do is move things away from them, so they don't hurt themselves.
If the overdose is patch-related, remove all patches from the skin immediately and carefully dispose of it.
There is a risk that opioid patches may be misused by others after their removal, so these need to be disposed of carefully. The used patch should be folded so that the adhesive sides stick to each other, wrapped (in paper for example) and disposed of in the garbage or a sharps medical-waste disposal container - out of reach of children.
For further information on where to get treatment and support for alcohol and other drug use, visit the Support & Treatment page.
For free and confidential advice 24/7 call Family Drug Support on
1300 368 186 or Alcohol and Drug Information Service (ADIS) on 1800 250 015. Counsellors are available to provide information, referrals, crisis counselling and support. Or start a
Web Chat with an ADIS counsellor online Monday to Friday, 8.30am – 5pm. ADIS can also provide up-to-date information about service availability in your area during the COVID-19 pandemic.
